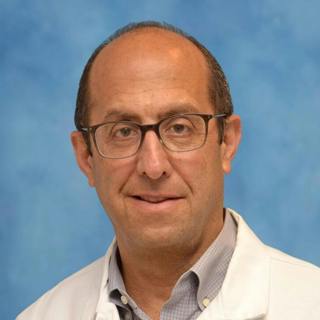
Ep. 390 Laser Atherectomy: An Overview of the Pathfinder Registry with Dr. Tony Das
In this episode of the BackTable Podcast, host Dr. Chris Beck discusses atherectomy, laser technologies, and their use in vessel treatment with Dr. Tony Das, an interventional cardiologist practicing in Dallas, TX and one of the founding members of the VIVA Vascular Education Course in Las Vegas. Dr. Das shares insights on the PATHFINDER registry, which is a prospective non-randomized, multicenter study to evaluate the performance and outcome of the Auryon laser atherectomy system. Their conversation explores the role of atherectomy in reducing stent usage, decreasing embolization likelihood, enhancing thrombus removal, and uncovering lesions. Dr. Das further provides recommendations for building a successful atherectomy program, utilizing laser technologies, and the importance of having ablative technology in outpatient labs. The doctors forecast future applications for artificial intelligence and remote monitoring. --- CHECK OUT OUR SPONSOR AngioDynamics Auryon System https://www.auryon-system.com/ --- SHOW NOTES 00:00 - Introduction 03:38 - Discussion about Connected Cardiovascular Care Associates 05:09 - Deep Dive into Atherectomy 14:06 - Understanding Laser Atherectomy 23:23 - Discussion on the PATHFINDER Study 34:52 - Advice for Building an Atherectomy Program 38:49 - Future Topics and Closing Remarks --- RESOURCES Connected Cardiovascular Care Associates: https://www.texasc3.com/ Pathfinder Registry Trial: https://www.clinicaltrials.gov/study/NCT04229563#publications Pathfinder Registry Trial Introduction: https://evtoday.com/articles/2021-sept/introduction-to-the-pathfinder-registry-and-complex-endovascular-cases-with-the-auryon-atherectomy-system Limb salvage following laser-assisted angioplasty for critical limb ischemia: results of the LACI multicenter trial: https://pubmed.ncbi.nlm.nih.gov/16445313/ Randomized controlled study of excimer laser atherectomy for treatment of femoropopliteal in-stent restenosis: initial results from the EXCITE ISR trial (EXCImer Laser Randomized Controlled Study for Treatment of FemoropopliTEal In-Stent Restenosis): https://pubmed.ncbi.nlm.nih.gov/25499305/ Cryoplasty Versus Conventional Balloon Angioplasty of the Femoropopliteal Artery in Diabetic Patients: Long-Term Results from a Prospective Randomized Single-Center Controlled Trial: https://link.springer.com/article/10.1007/s00270-010-9915-x#Abs1 Cryoplasty for the treatment of femoropopliteal arterial disease: results of a prospective, multicenter registry: https://pubmed.ncbi.nlm.nih.gov/16105918/ Auryon Laser from AngioDynamics: https://www.angiodynamics.com/product/auryon/ Philips Laser System: https://www.usa.philips.com/healthcare/product/HCIGTDPHLLSRSYSTM/laser-system-hcigtdphllsrsystm Atherectomy plus drug-coated balloon versus drug-coated balloon only for treatment of femoropopliteal artery lesions: A systematic review and meta-analysis: https://pubmed.ncbi.nlm.nih.gov/33478353/ Laser in Infrapopliteal and Popliteal Stenosis 2 Study (LIPS2): Long-Term Outcomes of Laser-Assisted Balloon Angioplasty Versus Balloon Angioplasty for Below Knee Peripheral Arterial Disease: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5407062/ Distal embolization during lower extremity endovascular interventions: https://pubmed.ncbi.nlm.nih.gov/28366300/ Shockwave™ Lithoplasty in Combination With Atherectomy in Treating Severe Calcified Femoropopliteal and Iliac Artery Disease: A Single-Center Experience: https://pubmed.ncbi.nlm.nih.gov/32563711/
4 Joulu 202342min

Ep. 389 Pelvic PT: An Introduction for Interventionalists with Ingrid Harm-Ernandes
In this episode of the BackTable Podcast, host Dr. Ally Baheti discusses the relationship between pelvic venous disease and physical therapy with Ingrid Harm-Ernandes, a pelvic floor physical therapist, mentor for Duke University’s Women’s Health Physical Therapy Residency Program, and author of The Musculoskeletal Mystery: How to Solve Your Pelvic Floor Symptoms. Ingrid gives a detailed walkthrough of a physical therapy session, highlighting the importance of holistic and interdisciplinary treatment approaches, as well as patient communication. She shares perspectives on the need for earlier interventions of physical therapy, misconceptions around the pelvic therapy issues, and the significant role of interventional radiologists as part of the treatment team. She also discusses her book which aims to demystify pelvic floor issues and empower both patients and practitioners in treating them. --- CHECK OUT OUR SPONSORS BD Advance Clinical Training & Education Program https://page.bd.com/Advance-Training-Program_Homepage.html RADPAD® Radiation Protection https://www.radpad.com/ --- SHOW NOTES 00:00 - Introduction 02:25 - Discussion on Pelvic Venous Disease and Physical Therapy 02:36 - Exploring the Role of Physical Therapy in Treating Pelvic Pain 04:41 - Understanding the Challenges in Treating Pelvic Pain 06:51 - Identifying Symptoms of Pelvic Venous Disease 10:06 - The Role of Pelvic PT in Treating Pelvic Venous Disease 15:49 - Finding a Qualified Pelvic PT 22:13 - Improving Synergy between Interventional Radiologists and Pelvic PT 28:39 - Understanding the Musculoskeletal Mystery in Pelvic Floor Symptoms 33:48 - Final Thoughts and Advice for Treating Patients with Pelvic Venous Disease --- RESOURCES The Musculoskeletal Mystery: How to Solve Your Pelvic Floor Symptoms: https://www.pelvicpain.org/resources/marketplace/books/the-musculoskeletal-mystery
1 Joulu 202337min

Ep. 388 Emergent Cases: The Impact of Arterial Sheath Technology with Dr. Rehan Quadri
In this episode, host Dr. Aaron Fritts interviews Dr. Rehan Quadri about the impact of intra-procedural arterial monitoring via sheath technology. Dr. Quadri is a practicing interventional radiologist at UT Southwestern in Dallas, Texas. --- CHECK OUT OUR SPONSOR Endophys https://endophys.com/ --- SHOW NOTES Dr. Quadri begins by telling us about a new arterial sheath, the EndoPhys Pressure Sense Arterial Sheath, which enables real-time blood pressure monitoring in a number of different cases and advantages that it offers over arterial lines and cuff monitors. We also discuss specific indications for utilizing this technology, such as trauma, GI bleeds, stroke, fistulas, and other emergent arterial interventions requiring minute-to-minute monitoring. We also breakdown the specs of the sheath, including its setup, calibration, placement, recorded measurements, and the accuracy of the read-outs when compared to those of past technologies. Dr. Quadri speaks on the cost and the overall value of the EndoPhys sheath. He concludes the episode by discussing new advancements in the technology such as improved device warmup times and a radial-specific sheath. --- RESOURCES Endophys Pressure Sense Arterial Sheath: https://endophys.com/
27 Marras 202331min

Ep. 387 Beyond BPH: PAE in Prostate Cancer with Dr. Nainesh Parikh
In this episode of BackTable, host Dr. Michael Barraza is joined by Dr. Nainesh Parikh from Moffitt Cancer Center. Dr. Parikh has worked extensively on prostate artery embolizations (PAE), having performed around 250 PAEs since joining Moffitt in 2017. The conversation delves into the multifaceted applications of PAE, with a specific focus on its role in prostate cancer. --- CHECK OUT OUR SPONSOR RADPAD® Radiation Protection https://www.radpad.com/ --- SHOW NOTES Dr. Parikh outlines the various clinical scenarios where PAE proves beneficial in prostate cancer cases. This includes the potential to shrink the prostate to an optimal size for brachytherapy, decrease volume for operational convenience, and address lower urinary tract symptoms associated with enlarged prostates. Clinical improvement emerges as a major motivator, with Dr. Parikh underscored the importance of ensuring a certain volume reduction before focal therapy, thereby simplifying subsequent treatments. The conversation extends to the role of PAE in managing radiation prostatitis, categorized clinically as chronic prostatitis. While conventional treatments often fall short for this condition, PAE emerges as an effective solution, especially for the 50% of men typically refractory to standard approaches. Dr. Parikh informs patients of the 70-75 percent chance of improvement while acknowledging the challenges in chronic prostatitis patients. The episode explores Dr. Parikh's approach to working up patients for PAE, with most referrals originating from the GU tumor board. Dr. Parikh discusses the gland size threshold for PAE assessment, emphasizing that while larger glands generally ease embolization, he occasionally considers PAE for smaller glands based on clinical context. Challenges associated with chronic prostatitis patients are acknowledged, with a focus on managing expectations due to a lower response rate compared to other PAE patients. Detailed insights into imaging protocols for follow-up are provided. For prostate cancer cases, Dr. Parikh recommends MRI at 6 and 12 weeks post procedure. He notes that there is notable reduction in PSA levels following PAE. Conversely, radiation prostatitis patients do not undergo post-procedural imaging unless PSA levels are detectable. As the episode concludes, Dr. Parikh highlights the future utility of PAE in prostate cancer, particularly in neoadjuvant settings before local or radiation therapy and even post radiation therapy.
24 Marras 202349min

Ep. 386 The PERT Approach: Innovating on Acute PE Management with Dr. Robert Lookstein
In this episode, host Dr. Chris Beck interviews Dr. Robert Lookstein about the pulmonary embolism response team (PERT) approach for treating acute pulmonary embolisms (PE). Dr. Lookstein is a practicing interventional radiologist in New York City at Mount Sinai Icahn School of Medicine. --- CHECK OUT OUR SPONSOR Penumbra Lightning Flash https://www.penumbrainc.com/products/lightning-flash/ --- SHOW NOTES We begin the episode by learning how Dr. Lookstein became involved in the PE space and how acute PE management has evolved. Dr. Lookstein breaks down the PERT at Mount Sinai, PERTs at other academic institutions, and the core qualities of a strong PERT. He walks us through a typical PE presentation, the process of PERT activation, and the workup with risk stratification. Dr. Lookstein also shares a few physical examination pearls for evaluating patients with PE and teasing out acuity vs. chronicity of presentation . Dr. Lookstein and Dr. Beck discuss endovascular PE interventions - ultrasound accelerated thrombolysis (trade name: EKOS catheter, Boston Scientific), first generation and second generation thrombectomy systems. The doctors also cover how advancements in technology have made these large-bore thrombectomy devices easier to learn about and use. Looking towards the horizon, Dr. Lookstein shares what we can expect from third generation technologies. We highlight how the primary endpoint of the PERT is to relieve the strain and stabilize/preserve the function of the right ventricle, regardless of how much clot is removed/remains. The doctors discuss the possibility of combined treatment algorithms for PE and the clinical data that has guided PERTs (all linked in resources below). To conclude the episode, Dr. Lookstein shares follow-up, longitudinal care, and how to tackle clot-in-transit. --- RESOURCES PERT Consortium: https://pertconsortium.org/ Ultima Trial: https://www.bostonscientific.com/en-EU/medical-specialties/vascular-surgery/venous-thromboembolism-portal/pulmonary-embolism/clinical-data/ultima.html HI-PEITHO Trial: https://www.bostonscientific.com/en-EU/medical-specialties/vascular-surgery/venous-thromboembolism-portal/pulmonary-embolism/clinical-data/hi-peitho.html CANARY Trial: https://www.acc.org/Latest-in-Cardiology/Clinical-Trials/2022/10/25/19/42/CANARY PE-TRACT Trial: https://evtoday.com/articles/2023-feb/pe-tract-a-closer-look STORM-PE Trial: https://pertconsortium.org/storm-pe-trial/ PEERLESS II Trial: https://ir.inarimedical.com/news-releases/news-release-details/inari-medical-announces-peerless-ii-randomized-controlled-trial
20 Marras 202359min

Ep. 385 Early (and Ongoing) Challenges in the OBL with Dr. Don Garbett (Live from WAIS)
17 Marras 202342min

Ep. 384 New Innovations in Closure Devices with Dr. Omar Saleh and Dr. Syed Hussain
In this episode, host Dr. Aaron Fritts interviews vascular surgeon Dr. Syed Hussain and interventional radiologist Dr. Omar Saleh about new innovations in closure devices. --- CHECK OUT OUR SPONSOR Vasorum https://www.vasorum.ie/ --- SHOW NOTES We begin the episode by discussing how closure devices have evolved over recent years and gained popularity in both hospital and OBL settings. Dr. Hussain and Dr. Saleh highlight the logistical advantages associated with a consistent, reliable closure device. Both doctors speak about their patients’ reported experiences and preferences for different types of closure devices and the importance of having a variety of options at hand. Dr. Saleh and Dr. Hussain also introduce the new CELT ACD closure device from Vasorum. We learn how to place a CELT, and Dr. Saleh highlights the ease of deployment and the reliability of results. Dr. Hussain also shares his experience in using the CELT, comparing its deployment to a “mic drop”. Additionally, we discuss if there are any potential drawbacks or special considerations that may exist in using CELT compared to other devices. The doctors cover the time from CELT closure to ambulation/discharge, citing an abstract published in Journal of Vascular Surgery (see resources below). Dr. Hussain and Dr. Saleh also report very few closure-site complications when using CELT, good outcomes with calcified arteries, and ease of bailout options. To conclude the episode, we discuss how physicians can get CELT and other products into their hospital or OBL through the Agency for Healthcare Research and Quality (AHRQ), Consumer Assessment of Healthcare Providers and Systems (CAHPS) scores, and other methods. --- RESOURCES Safety and Efficacy of the CELT ACD Femoral Arteriotomy Closure Device in the Office-based Laboratory: https://www.jvascsurg.org/article/S0741-5214(22)00945-4/fulltext Silent cerebral infarct after cardiac catheterization as detected by diffusion weighted Magnetic Resonance Imaging: a randomized comparison of radial and femoral arterial approaches: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1896179/ Vasorum CELT ACD Closure Device: https://www.vasorum.ie/
13 Marras 202354min

Ep. 383 Reflections on a Career in Clinical IR with Dr. Alan Matsumoto
In this episode of the "History of IR" series on BackTable, Dr. Alan Matsumoto, Chair of the Department of Radiology at the University of Virginia and a fellow of the Society of Interventional Radiology, joins our host Aparna Baheti. Dr. Matsumoto also serves as the Vice Chair of the American College of Radiology's Board of Chancellors. This installment provides a unique perspective on the life and career of Dr. Matsumoto and sheds light on the evolution of interventional radiology. --- CHECK OUT OUR SPONSORS Reflow Medical https://www.reflowmedical.com/ Medtronic Embolization https://www.medtronic.com/embolization --- SHOW NOTES Dr. Matsumoto's journey into IR commenced during his residency in the Department of Radiology at the University of North Carolina. The culture of independence within the department allowed him to gain extensive hands-on experience. Subsequently, after completing a four-year radiology residency followed by a one-year fellowship, Dr. Matsumoto ventured into private practice on the picturesque West Coast of Florida. However, his return to academic medicine was inspired by a profound appreciation for collaborative patient care discussions with referring physicians, marking a departure from the previous norm of merely appeasing them to maintain referral patterns. This transition led him to the University of Virginia, where he partnered with Dr. Tegtmeyer. Dr. Tegtmeyer's meticulous approach in running the IR suite, akin to a surgical suite, cultivated an appreciation for organizational precision and independence. During this conversation, Dr. Matsumoto fondly reminisces about Dr. Tegtmeyer, who emphasized the art of presenting oneself as an IR doctor to patients. He recognizes Dr. Tegtmeyer's passion for renal angioplasty, acknowledging him and Dr. Thoman Sos as pioneers in the field. Dr. Matsumoto also provides valuable insights into the technological landscape of IR in the past, underscoring the absence of contemporary tools like C-arms and pre-shaped catheters. Consequently, IR practitioners had to adapt and innovate, often crafting and modifying instruments, including innovative solutions like using styrofoam for embolizations or shaping catheters with bunsen burners. Furthermore, Dr. Matsumoto delves into the challenges faced by early practitioners, highlighting the need for caution to avoid detractors exploiting mistakes to diminish the value of IR procedures and potentially restrict the scope of IR practice. Balancing the role of a friendly collaborator with technicians and nurses while assuming leadership in the IR suite is a pivotal aspect of his journey. Dr. Matsumoto then elaborates on his pivotal involvement in aortic work in 1998, as he helped establish a core lab and collaborated with device companies along with CT and vascular surgeons. This work allowed him to be a part of the approval process of Medtronic’s AneuRx endograft in 1999, where he testified at the FDA hearing for this groundbreaking product designed to treat AAA’s. The transition to leadership within the department of IR at the University of Virginia marked another significant chapter in Dr. Matsumoto's career. Despite assuming this role unexpectedly after the passing of Dr. Tegtmire, he embraced the challenge. His vision for the department revolves around a heightened focus on clinical operations and streamlining patient responsibilities to enhance efficiency while upholding a culture of excellence. Dr. Matsumoto concludes this episode with valuable insights into strengthening an IR department by effectively promoting and communicating the value of services to the broader medical community.
10 Marras 202350min